Beauty
Your Period Could Change in Your 40s—Here’s How to Manage the Shift

Just as we are programmed to expect our first period with a combination of fear and panic, we also expect it to disappear. But the years leading up to menopause (which doesn’t officially start until you’ve been on your period for 12 consecutive months; the average age is 51) can, thanks to ongoing hormonal changes, present their own set of challenges.
These are challenges that many women, including this one, feel unprepared for. In a brutal twist, they often mirror what many of us went through as teenagers. “It’s like puberty, but at 40,” says Santa Monica ob/gyn Shamsa Amersi, MD. produced.”
And while we are becoming more and more familiar with the term perimenopause (defined as the transitional phase before menopause), there is still a lot of confusion about what happens to our bodies during this time, especially when it comes to our periods.
First, some basics: In a typical menstrual cycle, the ovaries produce a hormone called estrogen, which accumulates in the lining of the uterus, where a pregnancy can implant. In the middle of your cycle, you ovulate. When you ovulate, a mature follicle containing an egg is released, and if you don’t get pregnant, this triggers the production of the hormone progesterone, which aims to remove the uterine lining and also regulate your mood. (It is often referred to as the feel-good hormone.)
How does menstruation change in perimenopause?
As with adolescence, Dr. Amersi says, at 40, you may not ovulate every month. What does it mean? “You end up in a state of estrogen dominance,” Amersi explains, which thickens the lining of the uterus and can lead to what some of us unlovingly refer to as a crime scene period marked by copious discharge and intense pain. A drop in progesterone in your 40s can lead to a roller coaster mood as well as insomnia and sleep disturbance, all exacerbated by an overall concomitant drop in serotonin (the pleasure hormone).
What is a normal cycle?
To determine what constitutes a break in your cycle, it is important to understand what constitutes a so-called healthy period. “I always try to avoid the word ‘normal’ when talking to women who come to me worried about their periods because I don’t want anyone to feel abnormal,” says Cincinnati gynecologist and surgeon Somi Javid, MD. medical sciences. , from GerMD. when i’m a doctor Professionals describe menstrual cycles, Dr. Javid says, in terms of three factors: bleeding time, cycle length, and flow. “Typically women’s cycles are 7 days or less, cycle length can vary from 21 to 42 days, and discharge averages 4 to 5 pads or tampons per day,” she says. from measuring flow by consumption of a pad or tampon, and women simply state whether they find it abundant or not.
What many women begin to experience in their 40s is a change in the course, length, and length of their cycles. Some can be bloody while others are very light; some last longer and others not so long; some have a minor pain factor while others feel debilitating. That there will be some changes is inevitable, says Dr. Javid, although some changes should not be dismissed as typical.
“If your periods suddenly become very painful, last longer than 7 days, become severe, or occur less than once every 21 days, you should see your doctor for a physical examination and possibly lab tests and a pelvic ultrasound,” he adds. . Heavy bleeding can also be a sign of something more insidious, such as fibroids, polyps, cysts, adenomyosis, thyroid problems, bleeding disorders, or certain types of cancer, which is why many healthcare professionals advise women to use the app (Clue is great) to track your periods and monitor your symptoms.
Pregnancy, which more women are postponing into their 40s, can also disrupt your menstrual cycle because it essentially resets your endocrine (hormonal) and immune systems, says New York City-based holistic gynecologist Eden Fromberg, MD. post-pregnancy rhythms affect melatonin secretion, which is related to pacemaker control of the menstrual cycle,” explains Dr. Fromberg, adding that oxytocin and stress hormones are also affected by pregnancy and lactation, which can affect your cycle.
Recently, some people have reported changes in their menstrual cycle after receiving a COVID vaccine or becoming infected with COVID itself. Dr. Amersi notes that these hormonal changes typically last four to six weeks and do not affect fertility or the ability to conceive, although more research is needed on the effects of the vaccine on women.
Do hormonal contraceptives help or harm?
Women in their 40s who complain of heavy bleeding may be given birth control, which Dr. Amersi likens to putting a band-aid on their symptoms rather than addressing the root cause of the imbalance. “I always advise patients not to take birth control pills or synthetic hormones for an extended period of time due to risk factors for stroke, blood clots, and associated mood swings,” he adds. Dr. Fromberg agrees: “Long-term use of the pill can affect menstrual periods by recalibrating hormone receptors and hormone production in the endometrium, ovaries, pituitary, hypothalamus, and other tissues.
What does this mean for my skin?
Birth control or not, our skin can be a mirror image of our hormonal upheaval at 40. “The major hormonal changes that affect your discharge can also affect your skin,” says Dr. Javid. He explains that estrogen attracts water, so when levels drop, skin becomes drier. Collagen production is also reduced when estrogen does this, and acne is a common occurrence with hormonal cascades. When acupuncturist Sandra Chiu sees a new patient with any skin condition, she always asks and evaluates her menstrual cycle. “It gives us clues as to what might be wrong on the inside that could affect healthy skin function,” she says, adding that rosacea and melasma are problems she often sees in women in their 40s with disabilities. menstrual cycle.
Is there a way to make switching smoother?
There are ways to ease the hormonal transition at 40. And if you can start relaxing it sooner, that’s even better. “Developing healthy lifestyle habits in your 30s is important because each decade prepares you for the next,” says Dr. Amersi.
Chiu uses Traditional Chinese Medicine to treat patients in need of reproductive health and fertility support. “I think the more people who know that TCM can help with problems like painful periods, heavy bleeding, or cycle interruption without the use of birth control or pharmaceutical intervention, the more interest there will be in this option,” she says.
When it comes to diet, it’s especially important to consume sugar, alcohol, and gluten in moderation, as insulin resistance can develop in perimenopause, causing fatigue, insomnia, and hot flashes. Also make sure you’re getting enough protein (60 to 100 grams per day). “I’ve found that most of my female patients don’t get enough protein, and that can be a problem for hormonal health and even strong, healthy hair,” says Chiu. Good sleep hygiene and adequate hydration (from both water and food) are also key during this transition, Chiu says. While exercising, movement is vital, but consider replacing high-intensity cardio with strength training. “This approach is often more effective for reintegration and wellness than rapid exercise, which can overstimulate an already stressed adrenal and nervous system and compromise joint and structural integrity during a critical life transition,” says Dr. Fromberg.
What about additives?
There are a number of supplements that will help you maintain your hormone levels after 40. Dr. Fromberg recommends cimicifuga (a non-estrogenic herb), maca (root from the Andes), and vitex (also known as vitex) for symptom relief. “The fruit of Vitex agnus-castus, also known as vitex, especially increases luteinizing hormone levels, which can increase the luteal phase of the cycle as it declines during the menopausal transition,” says Dr. Fromberg. If you’re struggling with weight gain and fatigue, Dr. Amersi recommends adrenal support supplements such as ashwagandha, an Auruvedic adaptogenic herb. Michel Jacobs, co-founder of menopausal wellness brand Womaness, points to the effectiveness of Pycnogenol (French sea bark) both during and in the years leading up to menopause. “It can reduce pain associated with menstrual cramps, hot flashes, night sweats, and also help increase libido,” he says.
Any other support items worth knowing about?
Once empty, the market for vintage stamps continues to grow. Knix, Thinx, The Period Company, and Proof make great underwear for periods and leaks. “We created Proof as a solution for women of all ages, including women in their 40s who are experiencing unpredictable periods, postpartum urinary incontinence problems, and excessive sweating during exercise,” explains Proof co-founder Jody Kaden. Nyssa, a brand specifically designed for the postpartum period, has become a favorite for those who suffer from menstrual cramps: they make a pair of underwear with a bag that contains ice or a warm compress instead. Cora also makes a thin thermal patch that sticks easily to underwear. Another way to relieve cramps at home is Acera’s Lanshin massager, which uses infrared heat to relieve cramps while massaging the abdomen to stimulate blood flow. Preparing for something that can be wildly unpredictable can seem like a daunting task. “Perimenopause is clinically more challenging for patients in terms of symptoms than menopause,” says Dr. Amersi. It doesn’t help that there is no set time frame for change. “Women can be in perimenopause for varying lengths of time and it’s barely noticeable, or it can be eight years of slow change,” adds Jacobs. Accept the fact that change is coming, talk about it, and most importantly, ask for help.
Beauty
100+ Best Beauty Business Name Ideas

Even though there are many beauty business name ideas available, picking the right brand name can be tricky.
The beauty industry is fiercely competitive, so finding a unique name is one way to get noticed. But the question is, how do you choose the best one for your business?
Here’s our top list of name ideas for your beauty business:
- Catchy Beauty Business Name Ideas
- Unique Beauty Business Name Ideas
- One Word Beauty Business Names
- Creative Cosmetic Business Name Ideas
- Hair & Beauty Business Name Ideas
- Beauty & Wellness Business Names
- Health & Beauty Business Names
- Fashion & Beauty Business Name Ideas
- Business Name Ideas for a Natural Beauty Brand
- Classy Beauty Salon Names
- Mobile Beauty Business Names
- Cute Beauty Products Business Name Ideas
- Name Ideas for Clothes & Beauty Products
- Beauty Therapist Business Name Ideas
Catchy Beauty Business Name Ideas
- Beauty by [Your Name]
- The [Your Last Name] Beauty Salon
- [Your name] ‘s Beauty Store
- [Your name] ‘s Beauty Supply
- Beauty by Design
- The Beauty Studio
- Beautylicious
- Beauty Mark
- Polished
- The Beauty Spot
- Perfection
- Bombshell Beauty
- Pamper Me Pretty
- The Beauty Spot
- The Beauty Brigade
- Fabulous at Any Age
- Beauty by Design
- The Beauty Bar
- Pretty Please
- Beauty Junkies
- Beauty Secrets
- The Glamourous Life
- Couture Beauty
- The Beauty Connection
- Pretty in Pink
- Beauty Bliss
- Utopia
- Enchanted
- The Beauty Queen
- The Makeover Studio
- Beauty Oasis
- The Retreat
- The Femme Fatale
- The Bombshell
- The Glamazon
- The Femme Nikita
- Beauty Retreat
- Bare Escentuals
- Face Place
- Beauty Emporium
- Aqua Bling
- Beauty Boutique
- Pretty XO
- Eternal Youth
- Salon De Beaute
- Cutie Patootie
- Elegant Essence
- FormulaGlow
- Pretty Pulp
- Beautique
- Obey Your Beauty
- Pretty Fun
- Pool Noodle
- RetroCool
- EverGlowy
- TrueBeauty
- BeautyBuddies
- PrettyCherry
- PrettyPoppet
- Lucky Lipstick
- Wish U Were Here
- Sprinkles
- Pinch Me
- Escape
- Think Pink
- elly Be Thy Name
Unique Beauty Business Name Ideas
- Sweet Matter
- Self-Love Salon
- Bloom Beauty
- Diva Rose
- BeautyHour
- BeautyFable
- Lulla-Ladies
- BeautyBoard
- GleamGlow
- PrettyCrop
- Kitty Kisses
- New Age Beauty
- Modern Goddesses
- Nouveau Look
- Goddess Complexions
- La Femme
- TheRightPickUp
- BeautyRooms
- BeautyBlazer
- FancyFaceCo
- Mirror So
- Easy on the Eyes
- Bella Buzz
- The Glam Lab
- Inkwell Creative
- Skin Care Sundays
- Heavenly Goods
- Pretty Little Things
- BeautyDust
- Glam Rush
- TooGoodToGo
- DeLuxe It Up
- Blemishless
- Beauti-Full
- Dazzle Bubbly
- Tranquee
- Lilah Beauty
- Brillant
- Beau-Tiful
- Quietly Radiant
- Cover Queen
- You’re Lit
- Bold Minerals
- Club Queens
- Kendra Rose
- Heavenly Silks
- Hush Hour
- Beneath and Beyond
- Big Beauty
- Best of Your Skin
- Canvass
- Daisy and Daisy
- Eureka!
- Beautyalove
- Honeydew
- Pink Slip
- Tropical Pop
- Ivy and Mint
- Glowticity
Subscribe to Beautyholic!
Get updates on the latest posts and more from us straight to your inbox.SUBSCRIBEI consent to receiving emails and personalized ads.
One Word Beauty Business Names
- Siren
- Beautyology
- Venus
- Aphrodite
- Isis
- Cleopatra
- Nefertiti
- Allure
- Sultry
- Glam
- Luxe
- Chic
- Refined
- Timeless
- Opulent
- Splendid
- Glitz
- Fancy
- Flair
- Gleam
- Beautease
- Iridescence
- Scintillate
- Spark
- Dazzle
- Becauteous
- Glitter
- Radiance
- Beadazzled
- Lustrous
- Shine
- Resplendent
- Sheen
- Sleek
- Luminous
- Mystical
- BeautyBunch
- LuxeBeauti
- Mire
- Kyula
- Marron
- Treza
- Pique
- BareBeauty
- Beautlive
- Wildflower
- Honeybee
- She Cream
- GlowJo
- Fionull
- Cutera
- Neat-N-Even
- Layerly
- Glowy
- BerryNude
- Kalessie
- Lovelinesss
- Beautyify
- Rosebud
- Luxuriously
- Beautyous
- Bejeweled
- Onyx
- SkinMint
- Nailina
- Preen
- Quenche
- GetBeauty
- LuxReveal
- Eyelove
- Loveli
- Unblemished
- BeautyBae
- Beautypalooza
- Glamour Buzz
- Soulshine
- Dreamless
- Sweetz
- Moonfall
- Nailfection
- Lashique
- BeautyX
- Handsup
- Blushtease
- Naturess
- Vitalina
- BloomJewel
- CherIe
- TrendHead
- SweetPearl
- PearlIce
- PrettyMint
- SweetChin
- PrettySkin
- Spectabelle
- Zerobe
- Skinnia
- LaBelle
- Lalondon
- Vanitee
- Floris
- EyeLinx
- BeautyDome
- PinkTarte
- Cavale
- Entwine
- Bellita
- TotalGlow
- BeautySpot
- Glitterati
- Sweeten
- BeautyCall
- Beautica
- Magnetism
- Earthness

Creative Cosmetic Business Name Ideas
- Painted Lady
- Pretty in Pink
- The Cosmetic Kitchen
- Makeup Maven
- The Makeover Studio
- Dolled Up
- Color Me Beautiful
- Cosmetics & Co.
- Gorgeous Glam
- Makeover Magic
- Glamour Girl
- Color Dimension
- Lipstik Inc.
- Glossy Goals
- Cosmetic Secrets
- Coral Seashells
- Coralista
- Makeup Misfits
- FaceValue
- Beautitize
- Lipstick’s the New Nude
- Muddy Rose
- Cherry Lips
- Wet Aplenty
- Summer Scented
- Exfoli-tation
- Flower Scentsation
- RedsAndBombshells
- LusciousLips
- DestashingDiva
- DeGrasse
- Rosy Rose Petals
- Painted Paws
- PrimaLoss
- DeePressed
- NudeGloss
- Fantyx
- GirlyGloss
- NoMakeup
- Glitz n Glam
- Color Craze
- Playful Pout
- Plump Perfect
- Buttercream
- Powderish
- PowderFit
- Powdered
- BlankFace
- BareMarks
- MakeMePretty
- Rize
- Moodter
- Make Up Me
- Cheeky Charms
- AphroditeDerm
- UrbanLipstick
- LipsSoul
- MakeUpLife
- Acrystyle
- LipsWins
- GrinsLips
- MakeRose
- FacesNew
- BeautifulMist
- CosmeticsArt
- CosmeticsHazel
- Skinderella
- PoutBoutique
- Blush Buddy
- Lipstick Alter
- MakedUp
- BeautyBlisser
- Trumakeup
- Le Flawless
- Beautifyment
- LipMorph
- PowderCube
- Cosmeye
- Tristar
- MakeFine
- MaxLure
- Dabulous
- FlutterLash
- Mille and Haute
- StyleSand
- BeautyBot
- InfiniteChic
- Boudoir
- Smoked Lash
- Glam Stripe
- Hello Brights
- Nude You Makeup
- Chiquida
- Makeupia
- Snappy Sour
- Careful Darling
- Cosmetic Geek
- Sassy Shadow
- Boss Pretty
- Glamour Dolls
- Beautiful Kisses
- Kiss My Face
- MakeLab
- Lumicreamy
- Lasting love
- Short Sweetheart
- Lovers’ Kiss
- Hair & Beauty Business Name Ideas
- Cutting Edge
- Glossy Locks
- HairCurtain
- OliveYou
- KeratinDip
- Tressed to Impress
- The Mane Attraction
- The Cut
- A Cut Above
- Hair & Now
- Lashes & Locks
- Crowning Glory
- Curl Up and Dye
- Sugar Tressed
- Curl Custard
- Hairtreats
- Curl Blossoms
- Eve’s Garden
- Hair Carnival
- Hairstyles Unlimited
- Prima Donna Hair
- Fizz Hair
- Curls and Clicks
- Passion for Hair
- Hair Spills
- Make it Cut
- Love My Locks
- Facial Scissors
- Dye Shoppe
- HairSpa
- Locksmith
- Hair-iva
- Hairity
- Gypsy Hair
- All Hairs
- Haircuttery
- Hairlicious
- Beautyfuls
- Kera Care
- Hair Truths
- E-Luminate
- Hairpin Turn
- Lash Y’All
- Nooks and Knacks
- Twistspire
- Haircuttery
- Hairzz
- Beautyty
- Majestic Curls
- Haircut & Makeover
- Georgette’s Salon
- Hairsational Salon
- Braid Bar
- Dollish
- Knotty
- Dollin’ Around
- Hairspiration
- Curls N’ Quills
- Hair Hatches
- Hello, Handsome! Hair Parlour
- Hair Home
- Mane Attraction
- Curls & Company
- Love Your Length
- Curly Whiskers
- Beauty Splendor
- The Gleam Group
- Rocking Hair Salon
- Snip, Sip, and Style
- Hairitage
- Glow-Blow
- Bae-Stache
- Hair And Cuts
- Beautiful Hair
Why should you choose the best name for your beauty business?
A lot goes into selecting a name for your beauty or makeup business.
The biggest beauty brands usually have the most catchy and unique names. You can do this to make your business stand out from the crowd and attract clients.
Memorable names stick in people’s minds, which means they’re more likely to remember your company when they need your products.
Also, names that tell a story or carry a special meaning are especially effective.
A good name reflects your company well, so choosing one perfect for your brand is essential.
Whenever you decide to start your beauty company anywhere, come up with a name that will catch people’s attention.
How to come up with a beauty brand name?
Is your new beauty brand about to launch? Congratulations! It’s an exciting time for you and your business.
Whether you’re starting a small beauty shop or a new product line, naming is an essential part of success. Here are some tips for selecting the perfect beauty brand name.
Think about the meaning of your name
Is your brand all about natural beauty? Or maybe it’s focused on luxury and glamour?
Names should reflect what you sell and how you want to be perceived.
Choose a name that fits your brand’s feel and tone.
Check domain name availability
After you’ve come up with a few possible names, you should check if the domain name is still available. This is important because you want customers to be able to find your website easily.
Add a twist to it
Short and catchy names stick in your memory. Customers will remember your brand better when looking for beauty or makeup products.
Use SEO keywords
Your brand name should contain keywords that customers will likely use when searching for your products. It’ll help you show up on search engines.
Make it fun
When naming your business, don’t be afraid to get creative. Put your brain to work to come up with a name that stands out.
Seek feedback
The next step is to ask for feedback on the names you’ve come up with. Ask your friends, family, and even potential customers what they think of your name ideas. See which ones resonate the most and go with that.
Try a name generator
If you’re struggling to brainstorm names on your own, there are lots of online name generators that can help you come up with ideas for your new beauty brand and are free to use. Just enter a few keywords related to your brand, and you’ll get some names. Use keywords like ‘beauty store name’ or ‘beauty company name.’
Go with your gut
The bottom line is, you should pick a name that feels right to start your own beauty business. Trust your instincts and pick something that you’re proud of.
Over to you…
The sky is the limit when it comes to beauty business name ideas. The possibilities are endless.
But before settling on a name, think about what kind of brand you want to create. Do you want to create a luxury beauty brand? A natural beauty brand? A wellness beauty brand? Knowing where you want your brand to go will help you pick the perfect name for your business.
No matter what type of brand you ultimately decide to launch, we hope our list of makeup and beauty brand name ideas has given you some inspiration. Wish you luck!
Beauty
699 Original & Catchy Clothing Brand Names Ideas

Do you ever dream of starting your own clothing brand? It’s a lot of work, but it can be really rewarding. It’s fun to design clothes people love to wear. And you get to build a brand that represents your style and values.
So, if you want your clothing or a boutique business to be successful, give it a name that everyone will remember.
Here, we’ll explore unique clothing brand names that aren’t taken already so you can find your own.
- Cool Clothing Brand Name Ideas
- Unique Clothing Line Name Ideas
- Catchy Clothing Brand Name Ideas
- Exotic Clothing Brand Name Ideas
- Creative Clothing Line Names
- Luxury Clothing Names
- Traditional Names
- Urban Fashion Brand Name Ideas
- Vintage Ideas
- Plus Size
- Dog Clothes
- Baby Clothes
- Minimalist Brand Names
- Cute Clothing Brand Names
- Unique and Trendy Boutique Name Ideas
- Men’s Clothing
- Ladies Fashion
- Top Clothing Brand Names for Streetwear
- Sportswear
- Jeans
Cool Clothing Brand Name Ideas
- 21Story
- 24/7 Clothing
- Apparels 360
- Apparels Inc
- Attires Hill
- Blairs
- Couture Inc
- Couture Works
- Couturely
- Crene Crap
- Dolce Viva
- Fashion
- Fiesta
- Infinity
- Mad Colors
- Meta Cool
- Ninety Ninety’s
- Real Style
- ReVamp
- Studio9
- Style Archive
- Style Capsule
- Fashion Factory
- Style House
- Style Lab
- Suede Prime
- Style Yard
- The Cool Company
- The Couture Club
- The Shack
- The Style Club
- The Style Company
- Tiffanys
- Upstyle
- Urban Closet
- Vibe Store
- Vini Vidi
- Blue Chic
Unique Clothing Line Name Ideas
- 20/20
- 24 Karat
- Adaline’s
- Angels & Demons
- Archives
- Curves
- Euphoria
- Fleur
- French Closet
- Klothing
- Merci
- Milana
- OMG
- Penelope’s
- Riverdale
- Style Loft
- The Closet
- Très Chic
- Ubique
- Vogue
- Endless Rose
- De Novo
- Magnolia Boutique
- Sweet Repeats
- Forever New
- London Clothing Company
- Fashion Hub
- Living Simply
- Blueberry Hill
- Wear Classy
- Modern Appeal
- Unique Altered
- Primrose Shop
- 10 Days Apparel
- Zip & Buttons
- Florian Dress Shop
- Legacy Vintage
- Simply Wonderful
- The White Closet
- B&W
- Dolled Up
- Rewind
- Rack n Reroll
- Variation Vault
- This Year’s Gear
Catchy Clothing Brand Name Ideas
- Fashionista
- Threads & Trends
- Finders Keepers
- Belle Chic
- Aesthetics
- Suit Up!
- Fashionholic
- Cloud 9
- Big Bold Beautiful
- Beachy
- Abracadabra
- Bang On
- Dress R Us
- NY Wardrobe
- Sew in Style
- The Spotlight
- The Hanger
- Window Shop
- Fashion Week
- C’est la Vie
- Brooklyn 20-20
- Urban Apparels
- Seychelles
- Rehab
- Runway
- Night & Day
- Size Zero
- Knock Knock
- Viva la Vida
- Rock n Roll
- 80s Vibe
- Dots & Lines
- The Apparel Factory
- Sugar & Spice
Beauty
How can chin sculpting treatment help you?
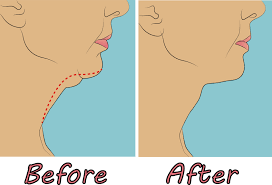
Chin sculpting is a treatment that uses PRP (platelet-rich plasma) and micro-needling to give you a slimmer, more defined jawline. The procedure can be performed in a single session and takes around two hours to complete. It’s suitable for all skin types and requires no downtime, so you can return to your busy schedule immediately after treatment.
A thin face shape is often linked to a stronger jawline.
You may find yourself longing for a more robust jawline if you have a thin face shape. A weak chin can make your face appear even slimmer than it is and make you feel like your face is too narrow. However, chin sculpting treatments can give you the look of a strong jawline without having to go under the knife or resort to injectables.
Chin sculpting treatment helps add definition and weight to your jawline so that it’s more proportional to the rest of your facial features. This works well for those who aren’t looking for significant changes but want their chin area to appear more robust than it currently does to balance out other aspects of their faces, such as oversize lips or high cheekbones that stand out more prominently than other features.
Sculpting your chin can make you look younger.
It can make you look younger. Not only does this procedure help patients achieve a more balanced facial appearance, but it also makes them look more attractive. This is because the chin plays a vital role in creating the face’s overall balance and harmony. These procedures are very safe and effective, focusing on reducing excess fat from under the chin area without causing any visible scars or wounds on your face.
You don’t have to worry about allergic reactions.
It is a non-invasive treatment that uses a laser to remove fat from the area around the chin, which helps reshape and contour it. It’s also known as laser lipolysis, but whatever you call it, this procedure has many advantages over traditional methods.
- No incisions or stitches
- No pain or recovery time
- No allergic reactions
Your face will look more balanced and attractive.
It can help you achieve a more balanced face. It is also known as chin augmentation or recontouring, and it can help you achieve that perfect balance between your lower and upper facial features. By restoring balance to your face, the overall aesthetics of your visage will appreciate greatly, and so will the way you feel about yourself.
The chin is vital in helping create visual harmony in the face; however, some people have chins that are too short, too long or need to be proportioned correctly with their other facial features (such as their nose). In these cases, chin reshaping surgery may be recommended to correct these issues by either making the jawline appear longer or adding definition to its shape through contouring techniques such as shaving down bone spurs from underneath skin areas above them (known colloquially as “fat grafting”).
If you’re looking for a new way to give yourself more confidence, chin sculpting could be the answer.
It is a non-surgical procedure that can help to reshape your chin, making it look more balanced and attractive. It can also make you look younger by eliminating excess skin on the neck and jawline, which often occurs with ageing.
The treatment involves strategically placed injections of hyaluronic acid filler or fat transfer to create a more defined jawline, balanced facial features and a youthful appearance. The patient may have some swelling and bruising following this procedure, but these will usually subside after a week.
It can be carried out under local anaesthetic or conscious sedation (where you are awake but relaxed), depending on each patient’s individual needs.
-

 Entertainment1 year ago
Entertainment1 year agoAdmiral casino biz login
-
 Entertainment2 years ago
Entertainment2 years agoHow Much Does The Rock Weigh
-

 Entertainment2 years ago
Entertainment2 years agoDownload Popular Latest Mp3 Ringtones for android and IOS mobiles
-
 Entertainment2 years ago
Entertainment2 years agoTop 10 Apps Like MediaBox HD for Android and iPhone
-

 LIFESTYLE2 years ago
LIFESTYLE2 years agoWhose Heartland?: The politics of place in a rural–urban interface
-

 Fashion3 years ago
Fashion3 years agoHow fashion rules the world
-

 Fashion Youth2 years ago
Fashion Youth2 years agoHow To Choose the Perfect Necklace for Her
-

 Fashion Today2 years ago
Fashion Today2 years agoDifferent Types Of lady purse






